The healthcare industry's response to evolving patient preferences and advances in technology has spurred the growth of virtual care and access to modern digital capabilities. And although paper medical records are being phased out in most healthcare settings – thanks to electronic health records (EHRs) – the current healthcare infrastructure lacks the support to address new challenges. This includes limited IT resources, siloed data across various systems, and rising patient expectations. Now the complete view of the patient is critical to deliver fast and efficient care.
But how? interoperability.
While the answer is simple, putting it into practice is more complex. Given that patients receive care from multiple providers across multiple healthcare systems, the smooth flow of patient data is crucial. Interoperability is the reason a patient can transmit their healthcare data from a Bluetooth-enabled pressure cuff to their provider's EHR, or how an emergency room physician can effortlessly retrieve test results from a patient's cardiologist with a simple click.
According to the Office of the National Coordinator (ONC), the United States has a goal to achieve nationwide healthcare interoperability by 2024. In other words, the U.S. aims to adopt a patient-centric system that can continuously improve care, public health, and science through real-time data access.
That said, if the nation is going to be anywhere close to meeting this goal in the next five years, healthcare organizations need to embrace interoperability and create a 360-degree view of their patients. With this, they can ensure and foster a system that empowers healthcare professionals, delivers visibility, and attends to patient needs in real time.
What is interoperability?
Think of interoperability as a universal language for different systems (e.g. software applications, third-party systems, electronic health records, and more) to communicate with one another. Primarily, it involves enabling the flow of information by breaking down data silos. Whereas integration provides the foundation for interoperability by connecting disparate systems, it frequently lacks the context of the information it brings together. By contrast, interoperable systems interact in the same language, minus the added delay or complexity. That way, healthcare providers and others can share critical information freely.
Particularly, information that is exchanged within interoperable systems follows the United States Core Data for Interoperability (USCDI v4) standards. This includes a diverse range of data: clinical notes, demographic information, medications, lab results, allergies and intolerances, and more. The list continues to grow as newer standards for data sharing emerges.
Although following interoperability standards can be a challenge, it's the key that allows organizations to function as a well-oiled, agile machine – and in healthcare, providing practitioners and patients a seamless experience.
Why is interoperability in healthcare important?
U.S. healthcare is a wide web of data, systems, and applications. Despite the majority of U.S. hospitals and office-based physicians implementing an EHR system of some kind, most involve fragmented data points and systems that are maintained by incompatible vendors. From dispersed patient files to scattered insurance data, this incompatibility results in clinicians having to time-consumingly piece together a complete view of the patient in order to provide the best care.
Simultaneously, there may be a resistance to change toward interoperability with the lack of standardization and inadequate technology infrastructure that exists in current healthcare organizations. All these shortcomings impact health outcomes and coordination efforts, including implementing a value-based care model, and is prompted by three challenges:
- Legacy health IT systems are increasingly incompatible with modern technology, causing delays in digital transformation. In fact, 64% of IT leaders identify legacy infrastructure, processes, and tools as a top barrier to transformation.
- System connections are driven by specific data requirements, resulting in a vast collection of point-to-point integrations. These integrations are costly to maintain and lack scalability across the organization, especially with 75% of U.S. hospitals managing more than 10 EHRs.
- Siloed patient data exists across clinical and non-clinical systems, creating disjointed experiences and missed opportunities for preventative healthcare (plus patient frustration). Despite recognizing the benefit of improved data quality and patient experiences through interoperability, many IT decision-makers struggle to connect data effectively. As a result, fewer than 40% of U.S. providers have successfully embraced interoperability to the point of efficiently sharing health data with other organizations.
Interoperability is the main goal, requiring the healthcare IT ecosystem to connect and transmit all necessary clinical and non-clinical information. Its significance lies in improving patient experiences, outcomes, and reducing readmissions. By easing the burden of disconnected data sources, interoperability also plays a crucial role in reducing clinician burnout and helping make fully informed care decisions. Ultimately, it enables the delivery of well-informed care, leading to the best possible outcomes for each patient.
Learn how to integrate your crm with your EHR
What are interoperability levels?
When it comes to healthcare interoperability, it's important to recognize that not all levels are equal. Let's consider the following levels: foundational, structural, semantic, and organizational.
Foundational
This level refers to basic standards needed for one information system to exchange data with another. Foundational interoperability serves as the bedrock, however, at this level, data information technology solutions are unable to interpret the received healthcare data on their own. To unlock its true value and derive meaningful insights, additional levels of interoperability are necessary.
Structural
This level defines the data structure of information (format, syntax, and organization) being shared between systems. With structural interoperability, data information technology solutions are empowered to effectively interpret the healthcare data they receive. However, it's important to note that while structured messages allow for interpretation, the lack of standardized content poses a challenge. This limitation curbs the potential for achieving higher levels of system understanding and integration between different healthcare systems.
Semantic
At this level, healthcare interoperability encompasses the integration of medical terminologies, nomenclatures, and ontologies, ensuring the effective sharing of medical concepts across diverse systems. Through semantic interoperability, data information technology solutions gain the ability to seamlessly exchange, interpret, and utilize healthcare data, unlocking its full potential for analysis and decision-making.
Organizational
This level encompasses governance, policy, social, legal, and organizational aspects, all aimed at facilitating secure, seamless, and timely exchange of healthcare data among various entities and individuals. It represents the ultimate objective toward which all healthcare organizations strive, and achieving this level requires shared processes and workflows that enables a smooth provision of healthcare across institutions.
Benefits of interoperability
Interoperability in healthcare has numerous benefits, the most obvious being that it provides all clinicians – no matter where they reside – a 360-degree, full view of their patients in order to make the most informed decisions in regards to their care.
Consider home-based care for patients with chronic conditions during the pandemic. Through interoperable medical devices, many patients were able to capture physiological parameters (e.g., weight, temperature, blood pressure, respiratory rate) and transmit this data wirelessly to their medical records. This enabled their providers to readily access and monitor this information, preventing the likelihood of patients being overlooked when stay-at-home orders were prevalent.
Healthcare interoperability also revolves around efficiency. For instance, enacting interoperability allows automatic appointment reminders or follow-up instructions sent directly to patients, besides physicians being able to transmit prescriptions directly to pharmacies. By optimizing time management throughout the entire spectrum of healthcare delivery, interoperability contributes to cost savings and improves health outcomes.
Healthcare interoperability minimizes the redundant collection of patient information. Imagine a situation where a hospital can receive insurance details from a patient's medical record while at a physician's office. This eliminates the need for patients to repeatedly retrieve and provide the same information. It also speeds up the billing process, ensuring that healthcare providers receive accurate payment from the outset and patients avoid receiving incorrect bills. What's more, it allows more time to be directed toward meaningful discussions regarding patient health concerns.
From preventing medication errors to stimulating consumer education and patient involvement in their own healthcare, the advantages of interoperability are endless. Without interoperability, we're left with higher medical costs, frustrated patients who are less likely to participate in preventive healthcare, and lack of trust in digital technologies.
Unifying patient data with EHR integration at Nebraska Medicine
Research shows IT teams spend 80% of their time on integration rather than innovation. As healthcare becomes more consumer-driven, the need for connected experiences grows, giving rise to more use cases for sophisticated, context-driven integration – the essence of true interoperability.
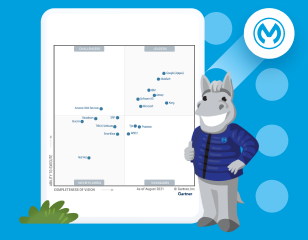
Nebraska Medicine, a prominent healthcare organization operating multiple hospitals, clinics, and specialty centers, recognized the importance of interoperability across their diverse locations. They turned to Salesforce and MuleSoft to enable seamless integration of their clinical and non-clinical systems.
By integrating Salesforce Health Cloud and EPIC with MuleSoft, they adopted an API-led approach that facilitated real-time data flow between systems, ensuring accurate and up-to-date patient records that were readily accessible to staff, and reducing cumbersome point-to-point integration. Over 110 staff and contact center agents now utilize Health Cloud, creating a comprehensive 360-degree view of the patient across all systems and significantly enhancing the quality of care, and a noted improvement to the employee experience who need to access these records as well.
What's more, in the first year of integration, they experienced enhanced agent productivity, leading to over $104K in realized savings along with over $376K in realized savings from one-call resolutions.
To implement a holistic approach to modern APIs for interoperability, learn more about how you can unlock the power of interoperability for your organization.